A robust, ready-made and cell-based cancer therapy inches closer to reality in light of recent progress. Researchers at the MD Anderson Cancer Center released results from their Phase I/II clinical trial on CAR Natural Killer (NK) therapy for blood cancers. The trial demonstrates encouraging patient responses to the treatment and identifies the best way to manufacture the cells to elicit positive outcomes.
What are Natural Killer Cells?
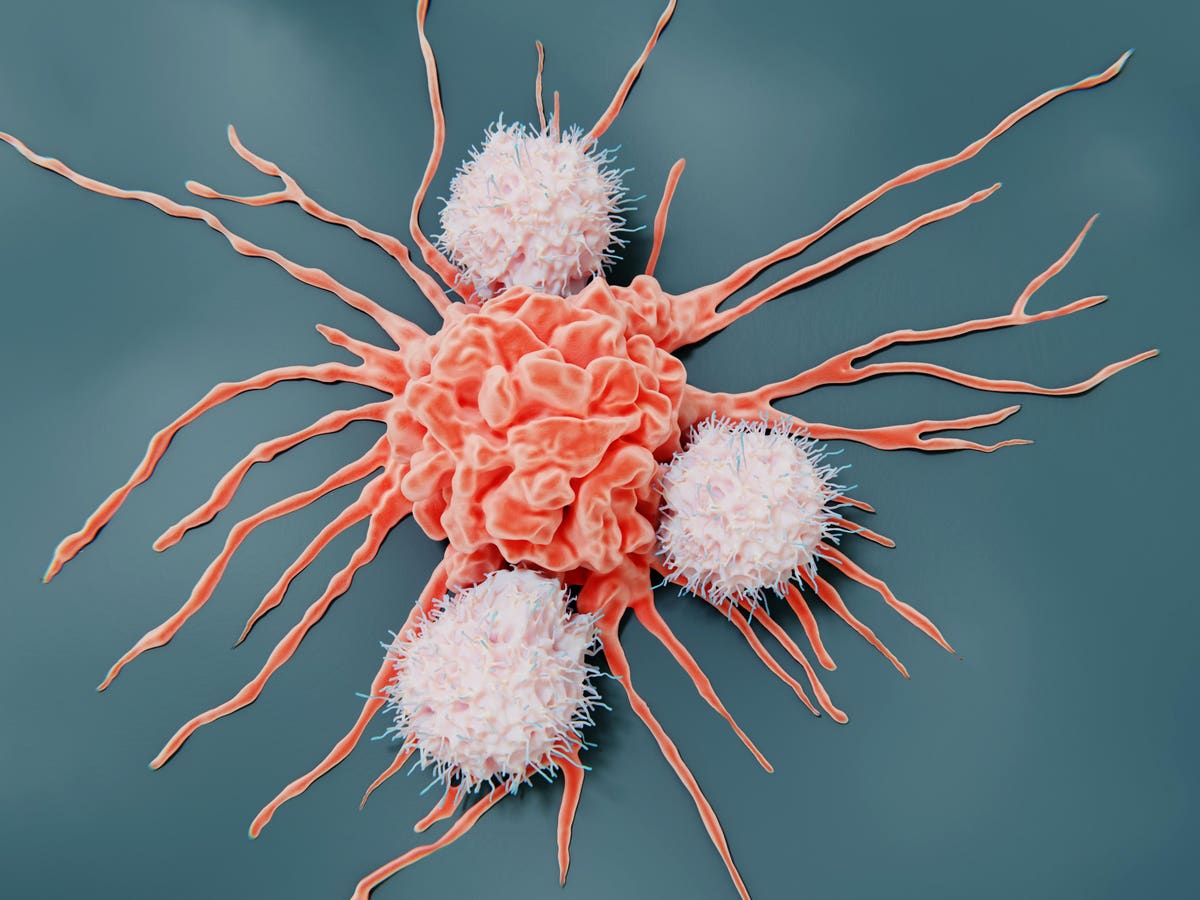
Natural Killer (NK) cells are white blood cells that can destroy infected, diseased and cancerous cells. They play a critical role in innate immunity, the body’s broad and primary defense against threats.
Natural killer cells earn their moniker because they do not require prior exposure to their targets to form their attack. Instead, they skim the cell surfaces of all cells that pass, initiating a sweeping search to determine if the cells are healthy or damaged. Cancer cells, hoping to avoid immune detection from CD8+T cells, will downregulate molecules known as major histocompatibility complex class I (MHC-I) on their surface. Natural killer cells can recognize this difference and strike—mainly by releasing cytotoxic enzymes, releasing immune chemicals called cytokines, or binding to a specific molecule on the target cell to trigger its cell death pathways.
The Appeal of Natural Killer Cells
Natural killer cells could represent a potent, safe and accessible alternative to conventional Chimeric Antigen Receptor T cell (CAR T) therapy.
Natural killer cells are inherently cytotoxic and possess several attack mechanisms. These cells are also prime candidates for donor-derived, scalable therapies, as they can be harvested from several sources, including peripheral blood, umbilical cord blood, and induced pluripotent stem cells. It would be cheaper to bulk manufacture off-the-shelf cell therapies than to continue with the industry standard: crafting a new cell infusion on a case–by–case basis.
Moreover, research suggests CAR NK therapy carries a low risk of cell rejection and potentially fatal adverse effects such as cytokine release syndrome. This favorable safety profile can likely be attributed to the unique cytokines expressed by NK cells and their ability to function independently of major histocompatibility complex binding.
Notably, CAR NK therapy patients must undergo lymphodepletion chemotherapy to prepare their bodies for the cell infusion. While a standard practice for CAR T therapy, the procedure depletes the patient’s immune cell counts and increases their risk of infection. This is an undeniable disadvantage; an ideal cell therapy would be affordable, readily available, and would not jeopardize the patient’s already compromised health with chemotherapy. (It is early days, but regulatory T cell therapy could one day treat cancer without preparatory chemotherapy; read more here).
Promising Clinical Trial Results
Would an allogeneic CAR NK therapy be safe and effective to treat cancer patients? To understand this, researchers at the MD Anderson Cancer Center in Texas enrolled 37 participants with blood cancers in their study.
In the dose-escalation phase of the study, eleven patients received increasing doses of CAR NK cells to determine the treatment’s maximum tolerated dose. Twenty-seven additional patients joined the subsequent study phase, which aimed to characterize the treatment’s toxicity and efficacy. The first twelve patients received CAR NK doses based on weight. The protocols eventually changed to give the remaining participants a flat amount of CAR NK cells; this should help patients adjust to an off-the-shelf product.
The team sourced their NK cells from umbilical cord blood. Cord blood is a rich source of immature natural killer cells. The blood can be conveniently collected, processed, and stored in advance—all attractive factors for more cost-effective and ready-made cell therapies.
The natural killer cells here wield a specific anti-CD19+ chimeric antigen receptor. The receptor expresses IL-15, a cytokine that improves NK cell expansion and persistence in the body, and inducible caspase-9, an enzyme that acts as the cell’s kill switch. If the therapy becomes too toxic, the researchers can activate the enzyme to destroy the CAR NK cells and cease the treatment.
Safety Profile and Response Rates
Overall, the patients responded well to the treatment. No one experienced graft versus host disease or neurotoxicity. One patient experienced mild cytokine release syndrome, a condition commonly associated with CAR T therapy. The preparatory chemotherapy temporarily depleted white blood cell counts, but this is an expected result. Finally, the maximum tolerated treatment dose did not cause unacceptable toxicity.
The treatment elicited a response in about half of the patients by Day 30; the team could not detect signs of cancer in 27% of patients in this cohort. By Day 100, more than a third of the cohort achieved a complete response. The durability of responses was evident, as patients who achieved complete remission by Day 30 showed a 70.0% probability of remaining in remission at Month 12.
CAR NK efficacy appears to vary depending on the blood cancer in question. For example, patients with low-grade non-Hodgkin lymphoma exhibited a 100% response rate on day 30 and an 83% complete response rate at Year 1.
The peripheral blood analyses reveal that patients who achieved an overall response demonstrate higher and longer persistence of CAR-NK cells in their blood. Notably, the degree of HLA mismatch with the recipient did not significantly impact CAR-NK cell persistence.
Insights on Manufacture
The team also analyzed cord blood to determine if any factors influenced the therapy’s success. They discovered that collecting and cryopreserving cord blood within the first 24 hours improves patient odds. To achieve optimal conditions, the nucleated red blood cell count also should not exceed 8 × 107 cells.
Future Implications
Although most cell therapies today are tailor-made to the patient, these resource-intensive protocols need to be simplified to reduce costs and improve access. To this end, trading killer T cells for natural killer cells may be a viable means of achieving a more cost-effective chimeric antigen receptor therapy.
This landmark clinical trial shows cord blood-derived CAR NK cells pose no immediate toxicities to patients with CD19+ blood cancers. However, the full extent of natural killer cells has yet to be revealed. More trial data is needed to determine if this therapy’s efficacy may one day surpass that of its counterpart, CAR T therapy. New adjustments could optimize the treatment’s design, such as integrating soluble IL-15 to prolong NK cell survival, administering multiple CAR NK doses for increased potency, or co-infusing NK cells alongside checkpoint inhibitors to improve their efficacy against solid tumors, a notoriously challenging obstacle for CAR therapies.
Read the full article here