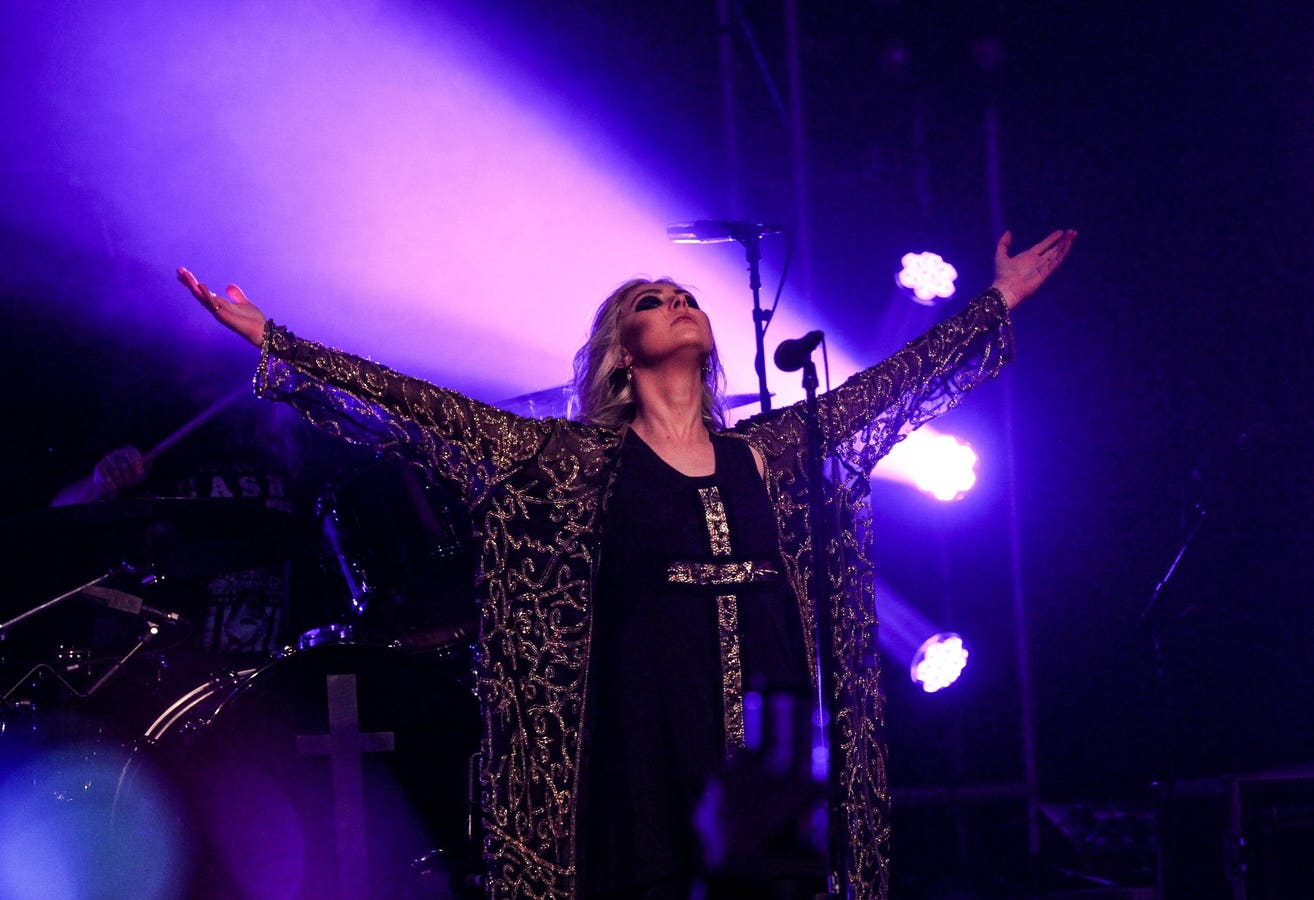
There’s a remarkable video of former Gossip Girl star and musician Taylor Momsen, who was bitten by a bat last week while she was performing. She was surprisingly calm after the audience pointed out a bat clinging to her thigh. She noted that she was performing “Witches Burn” at the time, as part of The Pretty Reckless opening act for AC/DC’s Power Up tour. Although she thought the bat was “cute,” it also “held on for dear life” as it was biting. She had to promptly go to receive treatment to prevent rabies.
Who’s At Risk For Rabies?
Rabies can occur following many mammal bites, most commonly those of bats, raccoons, skunks and foxes. Dogs are a significant risk for international travelers. In a 2019 study in Puerto Rico, 11% of cats tested were positive for rabies. The incidence of rabid animals has declined in the U.S. since 1990, although 4,000 cases are reported annually. More than 8 million doses of oral vaccines are distributed to animals through baited food.
Infections from bats that live in colonies are more common later in the summer when the young are learning to fly.
Those involved in an unprovoked attack from an animal should consider treatment. If the animal can be caught and quarantined, that is preferable; 10 days of quarantine is used for dogs and cats. Small mammals, like mice, chipmunks and squirrels, rarely transmit rabies.
A typical scenario is for someone to wake up and find a bat in their bedroom. They may well not know if they’ve been bitten or scratched, nor can a child, person with dementia or someone drunk reliably know. Such a fatal case in a 77-year-old woman occurred in 2016.
In the U.S., rabies prophylaxis is recommended in such a scenario. Because of cost considerations, in Canada, prophylaxis is only recommended if there is a known bat contact.
Per-patient median costs were $2,376 (with a range of $1,038 to $4,447) in Massachusetts in the 1990s. In 2018, a Georgia woman had to crowd-fund $10,000, for her treatment after a rabid bobcat attacked her.
Who Does Not Need Prophylaxis?
Since rabies is only transmitted through contact with saliva or brain/neurologic tissue, contact with blood, stool, urine or fur of a rabid animal is not enough to warrant prophylaxis.
Also, remember that the exposure to sunlight will kill the rabies virus. One study showed killing in 1.5 hours at 86 F with exposure to sunshine, but the virus was still alive at 20 hours without the sun. Drying it will also kill the virus, so inanimate objects an animal has touched are not usually a problem.
Rabies Treatment
First, the wound should be thoroughly cleaned with soap and water. Rabies immune globulin must be injected directly around the wound, and rabies vaccine must also be given that day and on days 3, 7 and 15 following the bite. [Tip: A friend was bitten by a rabid coyote as she got out of her car. The ER did not have her undress to examine her fully. When she got home, she discovered other bites and had to return to have more immune globulin injected around those. Insist that the staff actually examine you!] You should also receive a tetanus vaccine booster if you have not had one for several years, and may need antibiotics, depending on the bite.
I always had a low threshold for treating animal bites—rabies is almost 100% fatal if untreated and readily avoided with treatment. The first case of a death following post-exposure prophylaxis occurred last year in an 84-year-old man who was subsequently found to be immunocompromised. Insurance and health departments no longer consistently pay for this prophylaxis.
Note that there is a special warning to travelers—the quality of immune globulin or the storage conditions may not be as good in some less wealthy countries. Travelers exposed to rabies should consider evacuation back to the U.S. or have the treatment repeated upon their return.
Attitudes Toward Vaccination
In addition to the growing anti-vaccine sentiment fueled by misinformation through people like Robert F. Kennedy, Jr., there is spillover to people not wanting to vaccinate their pets. In a survey of 2,200 adults, “authors found that 37 percent of dog owners thought vaccines were unsafe for pets, 22 percent viewed vaccines as ineffective and 20 percent regarded them as unnecessary.”
Be more like Taylor Momsen. If bitten by an animal, seek medical care promptly. Rabies is preventable. So are many other infections.
Read the full article here