[NOTE: This article has spoiler alerts!]
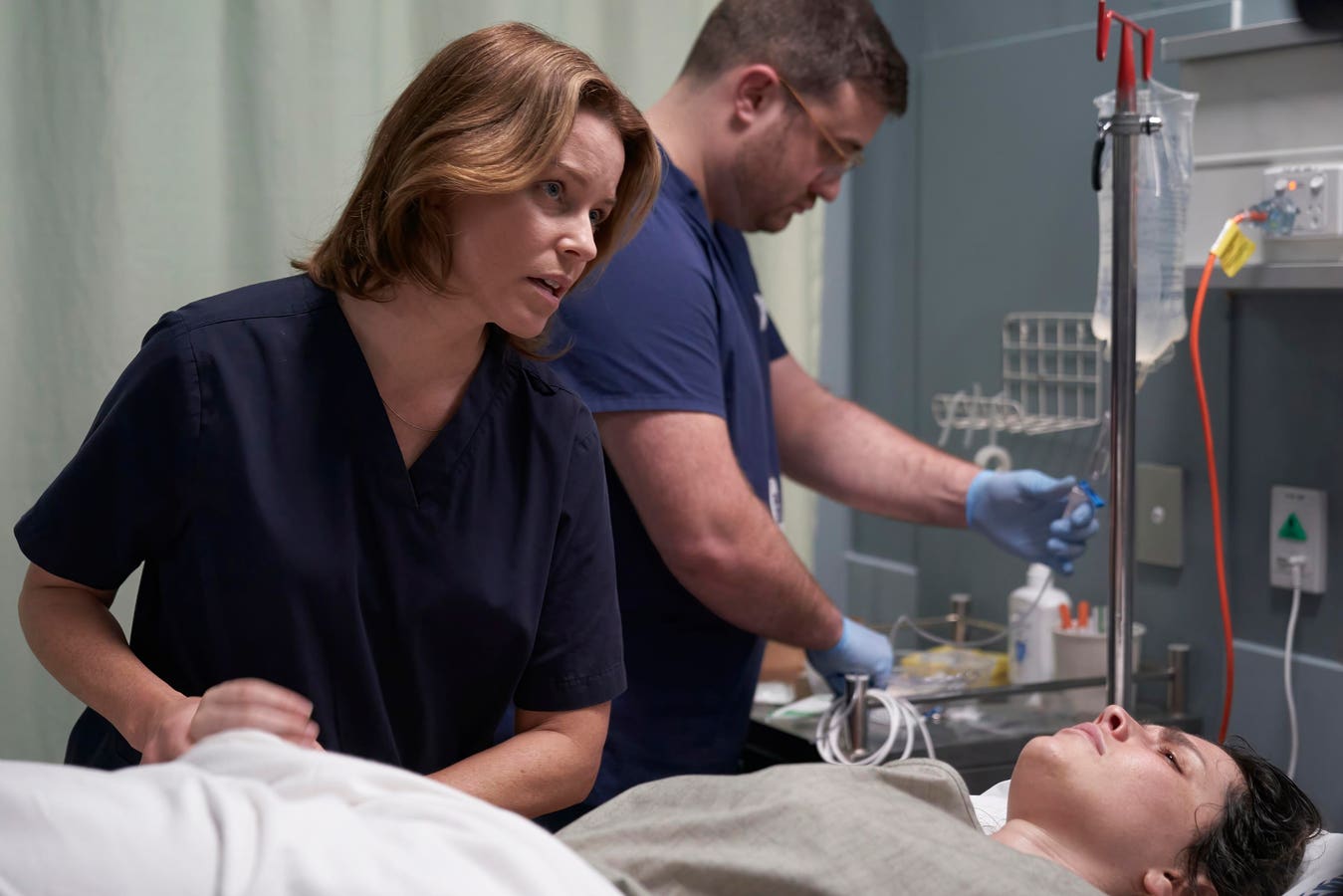
A Mistake is a captivating medical drama that premiered at this year’s Tribeca Festival. Set in New Zealand, the film tells the story of a surgeon, played brilliantly by Elizabeth Banks, whose resident, Richard, makes an error in the operating room. The subsequent fallout—tragic, political and sexist—pulls back the curtain on the gritty and unglamorous life of a doctor, the stressors of medical training and the emotional turmoil experienced by grieving families.
This film is not Grey’s Anatomy. Think of Apocalypse Now meets Terms of Endearment. As a female physician, I am grateful for director Christine Jeffs’ realistic portrayal of a surgeon’s life, particularly that of a female surgeon. A Mistake resonated with me on many levels. I’ll share my personal experiences as a woman doctor as well as my encounters navigating the U.S. healthcare system. I also interviewed two successful, high-achieving female surgeons who will also share their stories of grueling residency training complicated by gender bias and the demands of balancing surgical and domestic life.
When I asked Jeffs why she chose to make this film, she said the novel by the same name was brilliant. “Carl Shuker was an editor for the British Medical Journal for many years, so there’s so much truth in the actual details of the story, drawn from his extensive research,” explains Jeffs, who also directed Rain, Sylvia and Sunshine Cleaning.
Jeffs was also impressed by the strong female character: “It’s very important for me to present successful, vulnerable, real woman characters.” The New Zealand-born filmmaker was also shaped by her personal experience with the medical system, becoming an advocate for her partner “who was, through medical mishap, in a coma, in sepsis, dying. There was no pathway for him to survive that but he turned around.” Jeffs quickly realized the complexity of the healthcare system which she deftly portrays in A Mistake.
A Surgeon’s Life: A Realistic Portrayal
After the initial surprise of the New Zealand accents and lack of professional titles—the lead surgeon was referred to as “Mrs. Taylor” instead of “Dr. Taylor”—my memories of long hours, lack of sleep and the complexities of clinical care quickly rushed back. The film opens with Dr. Taylor sleeping in her scrubs a small bed in a dark room. Her phone rings; she answers and says “I’ll be there.” We then see her walking down a hallway, exhausted, towards the emergency department where she meets a frightened and ill-appearing young woman in pain. As she’s evaluating the patient, the attending surgeon is asking the resident questions while palpating the patient’s tender abdomen and providing bedside teaching, a key feature within all academic medical centers.
The above sequence brought back many memories of my own residency training: long hours, being on overnight call every fourth night (every third night if working in the intensive care unit), overwhelmed by sleep deprivation, being paged at all hours, addressing families’ questions, responding to ‘codes’ (e.g. cardiac arrest) and admitting new patients. Clinical teaching is also a key part of being a physician. We see Dr. Taylor frequently instructing her resident in the emergency department, in the operating room and even in a restaurant after-hours. The way she delivered her guidance in the latter scenario could have been better which I’ll get to later.
“Surgery is a great career and incredibly satisfying, especially when you see the immediate help you give patients and their families,” describes Jennifer Berumen, MD, a transplant surgeon at UC San Diego Health. “But when things go wrong, it can be devastating. It can be hard to remember the good things you have done.”
Surgery is an exceptionally demanding field. It takes a certain personality, says Alessandrina Freitas, MD, MPH, a plastic and reconstructive surgeon at White Plains Hospital.
“Surgery is not for everyone, and those of us that choose this lifestyle knowing the personal costs do so because it is our calling,” explains Dr. Freitas. “Being a surgeon is a core part of my identity and I would choose this pathway again. However, the stress is real: we are responsible for people’s lives in a very immediate and intimate way. Sometimes, you lose sleep over that. Sometimes things don’t go as planned.”
When Mistakes Happen
Doctors are not infallible. They make mistakes like all humans do. In the film, I felt that Dr. Taylor should have spoken to the family immediately after the operation and let her resident observe rather than leave it to Richard who was clearly uncomfortable and uncertain. Watching experienced attending physicians is how trainees learn. That said, when the lead surgeon did talk to the parents after the tragic loss of their daughter, the conversation could have been handled better. First, she should not have been alone but with a team including the ICU physician and nurse, a grief counselor and possibly the hospital chaplain. In addition, Dr. Taylor could have been more empathic using phrases like “sorry” and that their daughter “fought hard” and “wasn’t alone.”
The reality is that doctors receive very little formal guidance on proper communication during their many years of medical and surgical training. Dr. Freitas agrees.
“I received no direct ‘didactic type’ communication training, but I witnessed many examples of surgeons delivering grief-inducing news in both effective and terrible ways,” reflects Dr. Freitas. “I learned by witnessing and think that sometimes in surgery, training programs may exclude trainees from the difficult conversations. These conversations are critical to witness in training.”
The culture is changing, according to Dr. Berumen. “Medical schools now are doing more to focus on compassionate communication. In residency, there was very little focus on how to talk to patients and families, and a lot of focus on grinding through and just getting the work done.” She continued: “As a surgeon, knowing how to have tough conversations around complications and difficult decisions is incredibly important. If things are not initially handled well, patients and families won’t trust you as their surgeon.”
Double Standards Faced By Women Doctors
Women in all sectors face gender bias. The field of medicine is no different. Female physicians are often held to a different standard than their male counterparts, even down to clothing: one study showed that male doctors garnered respect regardless of their attire whereas most patients believed it was inappropriate when women physicians didn’t wear a white coat. Women doctors are also labeled “emotional” just like Banks’ lead surgeon whose boss, played sinfully well by Simon McBurney, showcased his misogyny further by stating that “women shouldn’t become surgeons.”
Dr. Berumen has witnessed gender-based discrimination throughout her career. “People call me ‘honey’ [but not her male colleagues], they comment on my appearance and ask if I’m pregnant.” She recalls male residents being invited to social events but not the female residents. The hepatobiliary surgeon also observed male attending surgeons sexually harassing female trainees. “One of my co-residents reported an incident, and no one believed her,” says Dr. Beruman. “A few years later, that male attending thatthe female resident reported was fired for the same sort of behavior.”
The double standards play out beyond hospital walls, too. I remember seeing a Broadway musical after my shift, still wearing a fleece vest with a hospital logo. A lovely man sitting next to me saw the medical attire, shared that he was a cancer survivor then asked, “Are you a social worker?” Many of my fellow female doctors are asked if they’re nurses, despite wearing a long white coat and a name tag displaying their physician credentials. Not my male colleagues. And this despite females making up over 55% of medical student enrollees. Gender-based discrimination is even worse among women physicians of color. Dr. Freitas has certainly observed double standards faced by female surgeons.
“Why do certain [male] surgeons get more support staff? Why do some surgeons rise through administrative ranks quickly?” asks Dr. Freitas, rhetorically. She has repeatedly witnessed favorable attitudes and achievements such as promotions granted to her male colleagues, and it’s “not because they are the most talented.”
While both Drs. Berumen and Freitas feel supported in their respective work environments, most female surgeons in the U.S. work in far more toxic spaces. Dr. Freitas asserts that “’emotional’ is a term to deride female surgeons.” She points out the double standard in how “women are ‘emotional’ but men are ‘passionate.’ I demand the very best for my patients. You can call it whatever emotion you want.” Dr. Freitas believes that the most effective way to handle gender-based discrimination is to point it out in real-time and move on.
My Take
As a female physician of color who has navigated the complex U.S. healthcare system from various clinical settings—academic medical centers, VA hospitals, homeless shelter-based clinics, Rikers Island jail and methadone clinics—I identified with Dr. Taylor’s frustration. The film depicts the difficulty in finding clear-cut answers in a field laden with nuance. A Mistake also underscores how women in medicine (all sectors, really) are constantly undermined by men (and sometimes women) in leadership positions. Not only was Dr. Taylor not “too emotional,” she displayed exceptional strength, taking responsibility for her resident’s error, living with financial independence and speaking up for her resident at his service.
I thought Jeffs did a great job humanizing doctors, revealing the multiple responsibilities they’re juggling at any given time (clinical, administrative, personal, educational, etc.) This delicate balancing act is further complicated for female physicians by workplace politics and gender bias. Doctors are not flawless, God-like figures. “We need to dissemble the narrative of the surgeon as a superhero because the effect is an unrealistic and unattainable goal,” declares Dr. Freitas.
After years of clinical medicine, I have learned that patients are ultimately seeking a desire to be heard. They want to know that doctors care, that we empathize with their pain, their frustration, their anger and confusion. They just don’t want to feel alone. Nobody does.
Read the full article here