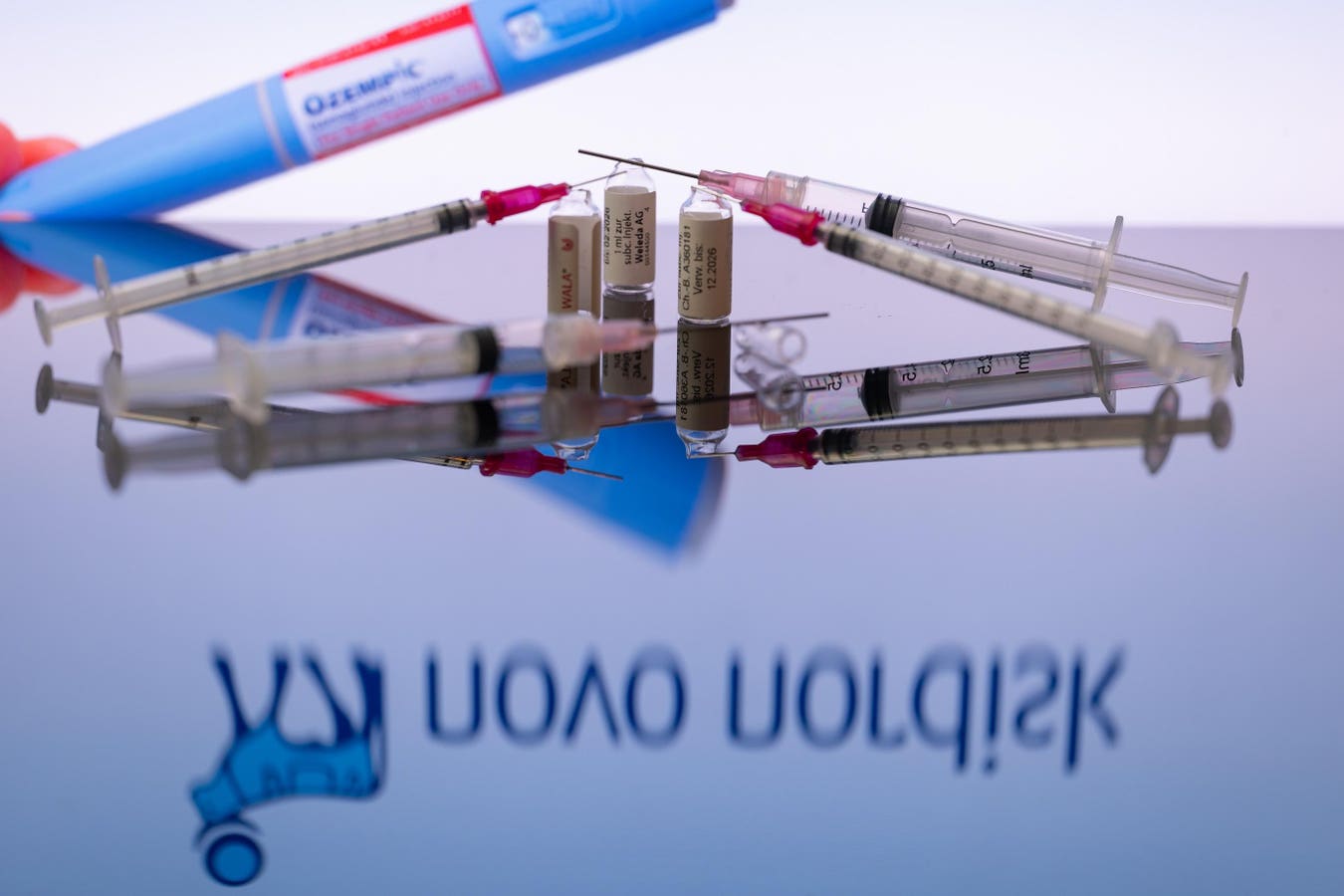
Weight-loss treatments like semaglutide (Ozempic) and tirzepatide (Mounjaro) have been game-changers for many individuals seeking to manage their weight. However, shortages and high costs have created significant barriers, prompting some patients to turn to compounded versions of these medications. But is using compounded Ozempic safe?
Here’s what you need to know
Compounded medications are custom-made to meet specific needs when standard prescriptions aren’t suitable. They are often prescribed when a particular medication, dose, or form isn’t commercially available. Compounding involves mixing precise amounts of active and inactive ingredients based on a doctor’s prescription, allowing for tailored solutions.
There are over 7,000 compounding pharmacies and over 35,000 active online pharmacies in the US. Generally, compounding a commercially available drug is not legal unless there’s a medical necessity, such as a shortage, discontinuation, or unusual dosage, or an alternate formulation is needed, such as a liquid formulation for those who have difficulty swallowing or to change the flavor for children. Additionally, if a patient is allergic to an inactive ingredient in a medication, a compounding pharmacist can produce the drug without that ingredient. It’s important to note that compounded drugs aren’t FDA-approved, raising safety and effectiveness concerns.
Stricter regulations were enacted in 2013 after a fungal meningitis outbreak linked to improper sterile compounding. To mitigate risks, compounding pharmacy accreditations have been established by the Pharmacy Compounding Accreditation Board (PCAB), the National Association of Boards of Pharmacy (NABP), and the Joint Commission. State Boards of Pharmacy may also regulate compounding pharmacies to ensure safety standards are met. Nevertheless, the FDA does not approve or monitor production of these medications.
Why are people turning to compounded Ozempic?
Some people may be turning to compounded Ozempic due to supply issues. Injectable GLP-1 medications, such as Ozempic and Mounjaro, have been in short supply since 2022. Affordability is another consideration, as the name-brand medications can cost $1,200 a month and may not be covered by insurance plans. Patients could expect to over $14,000 a year out-of-pocket, whereas compounded medications can be cheaper.
At my own weight loss practice seeing patients at Bariendo, I do occasionally prescribe GLP1 medications within certain parameters. For example, if a patient has had ESG Stomach Tightening performed, I may prescribe a medication temporarily to help optimize weight loss. A recent study indicates that weight loss medications are most effective when initiated within six months following ESG Stomach Tightening. This approach can lead to an average total weight loss of 24%. Therefore, it’s often advisable to undergo ESG Stomach Tightening first. At present, we only prescribe brand-name medications such as Wegovy, Saxenda, Ozempic, Mounjaro, and Zepbound and do not use compounded pharmacies with our patients.
The FDA allows the compounding of patented drugs like Ozempic and Mounjaro only when there’s an official shortage, as is currently the case with semaglutide and tirzepatide. Despite this, compounded drugs are not the same as FDA-approved medications. While the FDA can authorize a drug for compounding, it does not oversee the production process or test the final product for safety and efficacy.
FDA warning about compounded Ozempic
In January 2024, the FDA posted a statement cautioning against the use of compounded semaglutide when the approved version is available. The agency again highlighted that it does not review compounded drugs for safety, effectiveness, or quality, and has received adverse reports from patients using compounded semaglutide.
Novo Nordisk, the only FDA-approved manufacturer of semaglutide, does not sell the active ingredient to compounding pharmacies. Some compounders may be using salt forms of semaglutide, which are different from the active ingredient used in approved drugs like Ozempic and Wegovy.
The FDA warned: “The salt forms are different active ingredients than is used in the approved drugs, which contain the base form of semaglutide. The agency is not aware of any basis for compounding using the salt forms that would meet the FD&C requirements for types of active ingredients that can be compounded.”
This lack of oversight and potential use of unapproved ingredients can lead to serious consequences, including contamination or incorrect dosages. The FDA has warned that some compounding pharmacies use unapproved starting ingredients, leading to potential adverse events.
The National Association of Boards of Pharmacy states that only about 5% of the 35,000 active online pharmacies comply with U.S. pharmacy laws and practice standards. This means that many compounded medications might not meet essential safety and efficacy criteria.
Unsafe drugs sicken patients
Last year, three individuals in the United States were hospitalized due to dangerously low blood sugar levels, linked to counterfeit versions of Novo Nordisk’s Ozempic, according to the American Association of Poison Control Centers (AAPCC) as reported by Reuters.
Throughout the year, the AAPCC recorded 3,316 calls related to semaglutide, the active component in Ozempic. This figure is more than double the previous year’s calls and represents a 15-fold increase since 2019, CNN reported.
Most of these calls were due to severe side effects commonly associated with semaglutide, such as nausea, vomiting, and stomach pain, which were typically managed with intravenous fluids and anti-nausea medications.
In the three severe cases of hypoglycemia, or low blood sugar, the AAPCC suspected the presence of counterfeit semaglutide. These incidents were all reported by the same regional poison control center, one of the 55 in the U.S., according to Reuters.
Additionally, last year saw a case of hypoglycemia in a user of a compounded version of Ozempic in the U.S. The FDA has noted that during drug shortages, such as the one affecting Ozempic, qualified pharmacies are allowed to create compounded versions. However, these versions are not subject to the rigorous testing and controls that branded medications undergo, making them potentially unreliable.
Ensuring medication safety
Consumers need to exercise caution when considering compounded medications. Additionally, extraordinarily low prices are often too good to be true and may indicate substandard or counterfeit products.
To verify the legitimacy of a compounding pharmacy, patients can use the FDA’s BeSafeRX program, which helps identify licensed and certified pharmacies.
Read the full article here