A Centers for Medicare and Medicaid decision memorandum issued last month lifts restrictions on coverage of Alzheimer’s disease diagnostics that measure beta amyloid plaque in the brain. Excessive levels of plaque are considered an indicator of the presence of Alzheimer’s disease. Facilitating reimbursement of diagnostic tests is critical in light of recent approvals of drugs intended to reduce amyloid plaque. But questions remain regarding equitable access, as coverage decisions will now be made at the local level by Medicare Administrative Contractors.
Alzheimer’s disease is the most common cause of dementia, accounting for 60-80% of all cases in the U.S. It is clinically diagnosed based on the presence of cognitive impairment that severely interferes with the activities of daily living.
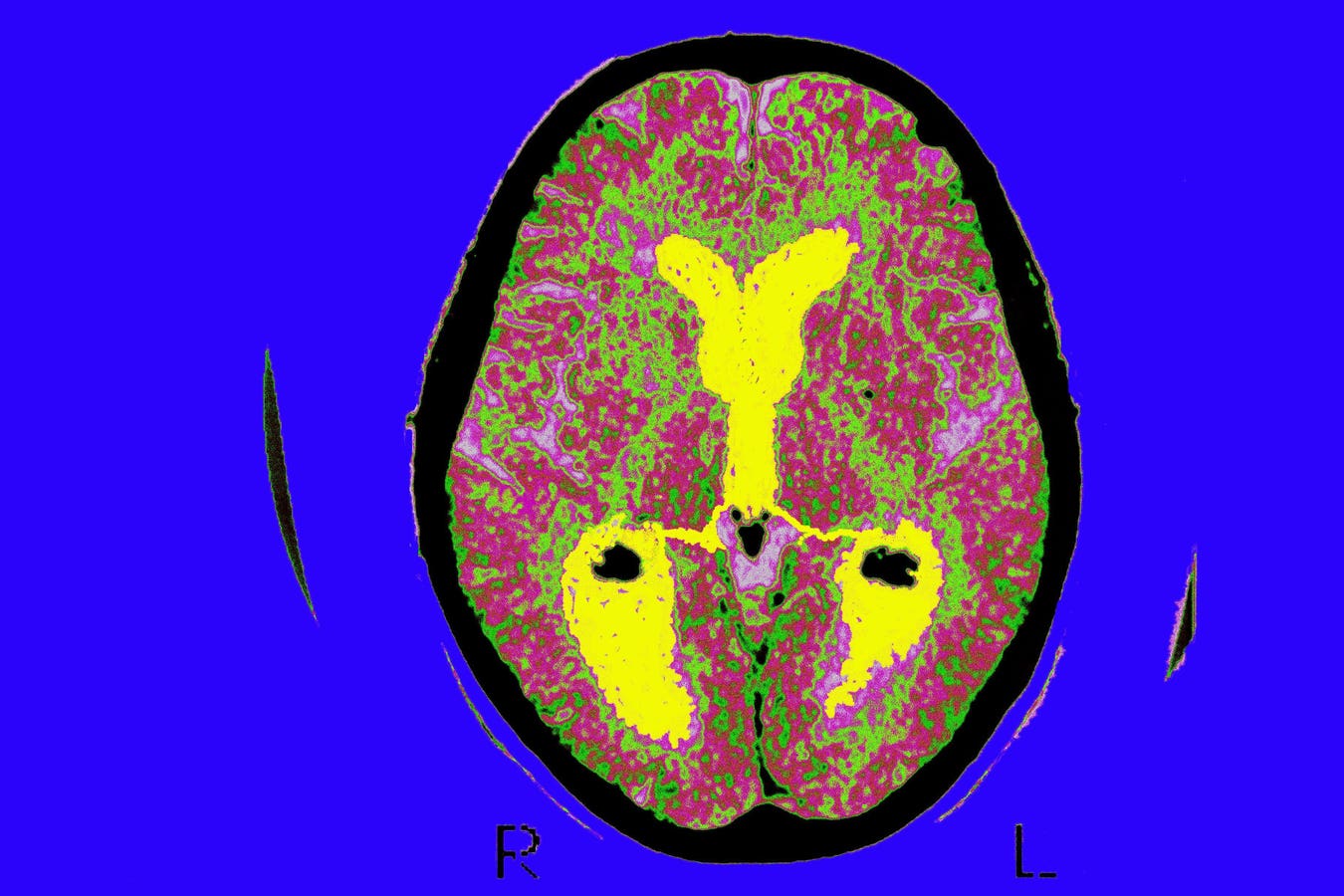
A pathological diagnosis of Alzheimer’s disease is possible after verification of the presence of beta amyloid plaques in brain tissue. Beta amyloid is a naturally occurring protein. Abnormal levels of it clump together to form plaques that collect between neurons and disrupt cell function, which in turn can lead to cognitive decline.
Thanks to several products launched a decade ago there are diagnostic tools to evaluate beta amyloid density. In 2012, florbetapir 18F—marketed as Amyvid—became the first diagnostic agent to be approved by the Food and Drug Administration for positron emission tomography of the brain to assess plaque build-up. Subsequently two similar PET agents, flutemetamol 18F and florbetaben 18F were approved.
Knowledge gained from amyloid PET scans informs clinical decision-making by potentially preventing misdiagnosis and reducing the risk to patients of adverse treatment effects.
But soon after their approval, Medicare issued a National Coverage Determination in 2013 which severely restricted coverage of these scans to patients enrolled in so-called coverage with evidence development programs. Specifically, patients had to be part of an authorized clinical trial—preferably a randomized controlled study—to examine “evidentiary gaps” in the usage of such scans, particularly with respect to how they potentially improve health outcomes. In addition, patients could only have one reimbursed one beta-amyloid PET scan.
The decision by CMS in October to end the coverage with evidence development program constitutes an improvement in access to beta amyloid imaging tools for Alzheimer’s disease patients.
It makes sense that CMS changed its policy given the recent approvals of drugs which are designed to remove beta amyloid plaque: Aduhelm (aducanumab) and Leqembi (lecanemab). Immediately following Leqembi’s regular approval by the FDA in July, CMS announced it would cover much of the cost for most patients who are eligible for the therapeutic. This includes patients with mild cognitive impairment or mild dementia with confirmed amyloid plaques.
In order to benefit from these biologic therapeutics patients must have beta amyloid plaque present in their brains. It would therefore seem imperative that Medicare beneficiaries prescribed, say, Leqembi, are all provided reimbursed access to multiple amyloid PET scans to assess possible reductions in plaque levels over time.
The need for universal access is amplified by the CMS requirement that Medicare beneficiaries who take Leqembi enroll in a patient registry to collect more data on the drug’s safety and effectiveness. In turn this evidence gathering will invariably include widespread use of PET scans, not only for diagnosis but also follow-up care.
However, CMS now leaves coverage decisions up to local reimbursement authorities called Medicare Administrative Contractors. Granted, in Medicare most coverage decisions regarding prescription drugs, diagnostics and medical devices are made locally or regionally. But this can yield inequities in the system as significant variation in coverage may occur across different insurance carriers. With certain ethnic groups like African Americans and Hispanics at greater risk of being diagnosed with Alzheimer’s, it’s especially important to minimize discrepancy in the coverage of amyloid PET imaging.
Read the full article here