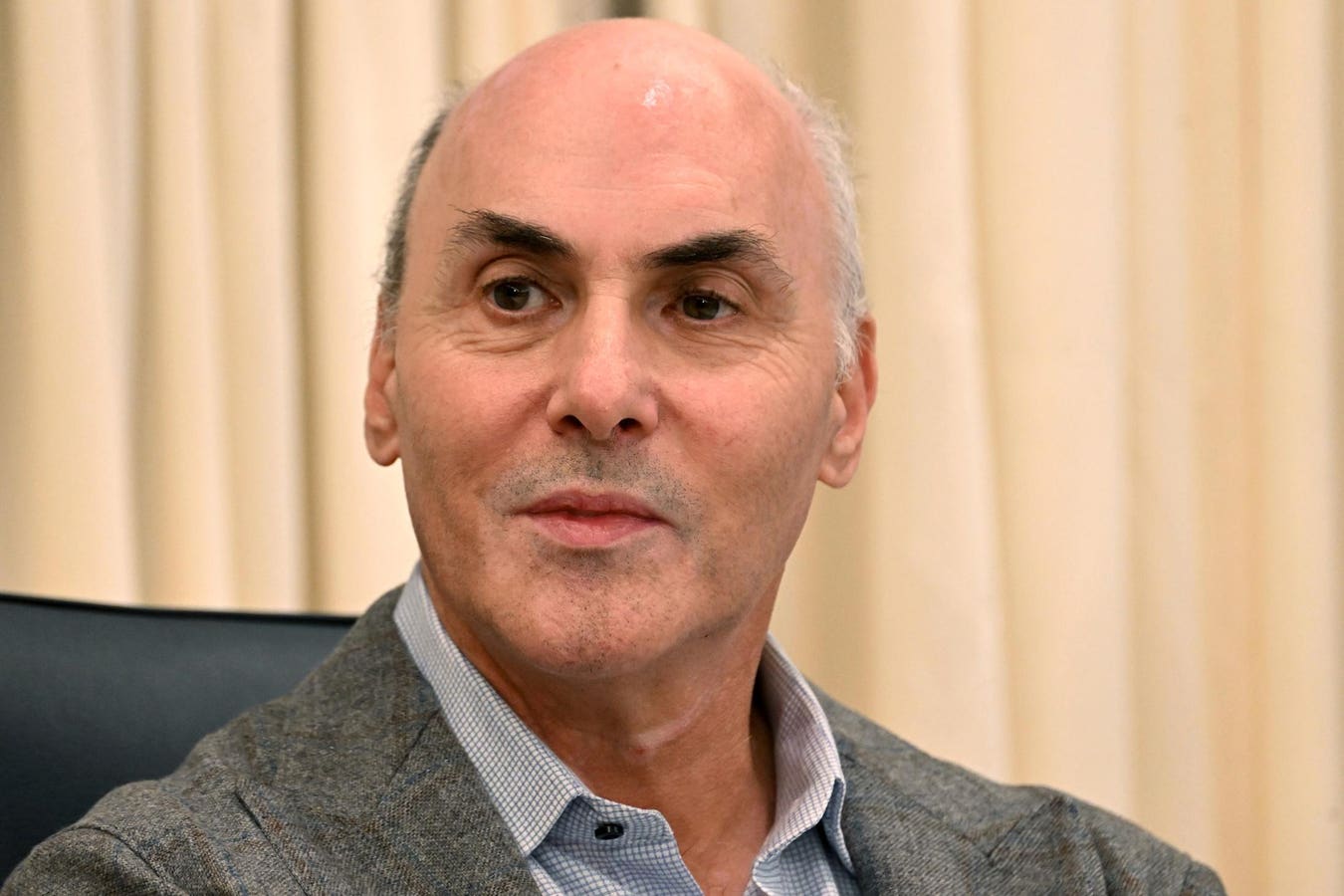
If you, like me, are among the several billion people who received an mRNA Covid-19 vaccine, we have benefited from one of the greatest medical breakthroughs in human history. And we have many scientists to thank, including American physician and immunologist Drew Weissman, who shared this year’s Nobel Prize in Physiology or Medicine with his research partner Katalin Karikó. Last week, I had the honor of speaking to Weissman about how he envisions the future of mRNA vaccines and therapies.
For quick background, Weissman and Karikó spent years solving the incredibly complex problem of how to dampen the harmful effect of lab-made mRNAs on the immune system. In a landmark paper in 2005 in the journal Immunity, they reported that a substitution of one chemical base of the mRNA molecule for another modified base nearly eliminated the immune reaction. Several of their later papers showed that the modified mRNA also greatly increased protein production compared to unmodified mRNA.
Their breakthrough helped lay the foundation for the Covid-19 vaccines, which cleverly train our bodies to prepare to fight the virus without seeing the real thing. As the Nobel Assembly wrote in its announcement of this year’s award, “Through their groundbreaking findings, which have fundamentally changed our understanding of how mRNA interacts with our immune system, the laureates contributed to the unprecedented rate of vaccine development during one of the greatest threats to human health in modern times.”
Weissman is a quintessential scientist: humble, matter of fact, driven and not content to rest on his laurels. Rather, he’s laser-focused on working to alleviate devastating diseases “that torture the human race.” Our discussion revealed seven memorable insights:
1. Many of our new vaccines will be RNA-based, but not all.
“All of the more difficult diseases, RNA is leading the development, so for HIV, Hepatitis C, TB, malaria,” Weissman said. “RNA vaccines are now in clinical trials for all of those.”
For common diseases, it’s hard to replace an established, cheap technology that is easy to distribute around the world with something new. “The MMR vaccine, for example, is dollars to produce and works great. I don’t think that is ever going to be replaced with RNA or if it is, it will be a long time coming.”
2. Beyond vaccines, there’s tremendous momentum to develop mRNA therapies for noninfectious diseases, including genetic and autoimmune diseases and cancer.
There are many diseases in which the body does not produce the right protein or enzyme, and which may theoretically be corrected by mRNA being sent to the right organ or cell to replace the malfunctioning one with the right copy. Thanks to Weissman and Karikó’s discovery of figuring out how to enable the body to tolerate lab-made mRNA without a prohibitive immune reaction, the race is on to develop potentially curative therapies not possible until now.
3. The future of gene therapy depends on targeted delivery, which Weissman is working on.
By now, most people have heard of lipid nanoparticles, the fatty delivery vehicle that stabilizes fragile mRNA. The thing about LNPs is that they go to the liver, because the liver has blood vessels with larger pores that attract these nanoparticles. This is a great approach for liver diseases, but not as helpful for all the diseases that originate in other places outside the liver.
“We figured out how to target LNPs to other cells and tissues,” Weissman told me. “We had a paper in Science a few weeks ago where we targeted repopulating bone marrow stem cells with incredibly high efficiency approaching 100% for gene editing.”
He’s working with other researchers, including the Gates Foundation, to develop several novel approaches to curing sickle cell disease.
“The future is going to be, we can go to Africa and the entire world, give people a single injection of RNA LNPs that are targeted to bone marrow stem cells and correct the gene mutation for sickle cell and cure sickle cell with just a simple injection.”
He adds: “You can expand that to the thousands of other bone marrow and genetic diseases. We can also target brain, lung, heart, kidneys, spleen, adrenals, and we continue to expand that. We’re working on being able to deliver either therapeutic proteins or gene editing technology to a variety of diseased cells or tissues.”
4. Faster, easier and cheaper CAR T-cell therapy is a major challenge that Weissman is working on.
Back in 2010, the first cancer patients were treated with CAR T-cell therapy in a landmark trial at the University of Pennsylvania Perelman School of Medicine (where Weissman also has his lab). The first child ever given the therapy, Emily Whitehead, went into remission from leukemia and is still doing well today.
The therapy works by removing some of a patient’s own T cells, engineering them in a lab to hunt down their cancer, and then infusing the souped-up T cells back into their bodies to circulate in perpetuity as a living drug.
So far, there are five FDA approved CAR T-cell therapies, all for hematologic malignancies like leukemia and lymphoma. To date, 27,000 patients worldwide have received approved CAR T-cell therapies, not including clinical trials. But the time, cost and complexity to engineer a patient’s own cells outside their body puts the therapy out of reach for many.
One of the next horizons is to figure out how to engineer the cells inside a patient’s body, known as in vivo—a much more direct and efficient approach. Weissman is working on targeted T-cell delivery of RNA therapies.
“We’ve shown in our cardiac fibrosis paper that we can cure a mouse with a single treatment,” he said.
Clinical trials for in vivo CAR therapies are expected to start within a year or two, and the earliest FDA approval would be a few more years after that.
5. Figuring out how to make CAR T-cell therapies attack solid tumors—which make up 90% of adult cancers—is a significant unsolved problem.
“I suspect it will be a multistep process,” Weissman said, “because there are lots of issues with solid tumors. The environments are immunosuppressive,” so even if the cell therapy gets into the tumor, it gets turned off and can’t kill the cancer.
Different approaches under study include adding proteins or knocking out proteins to make the CAR Ts more functional, including with gene editing. “Many levels have to be addressed before we come up with something that works well.”
6. Weissman is developing new vaccines and the basic science underlying them.
His lab has a couple of HIV vaccines and universal influenza vaccines in clinical trials, as well as a pan coronavirus vaccine that will go into clinical trials soon.
7. The time is coming closer for personalized cancer vaccines.
“There are already cancer vaccines in clinical trials that have shown efficacy for melanoma and pancreatic cancer,” Weissman said. “They are in phase 2 now, I’m sure they will move to phase 3 very quickly and they’re continuing to study many other types of cancer with personalized vaccines.”
Looking Ahead
Thanks in part to Weissman and Karikó’s breakthrough, there are close to 1,000 approaches in development for new vaccines and therapies using mRNA. (Disclosure: One such example is Capstan Therapeutics, a startup co-founded by Weissman and which has received an investment from my team at Leaps. Capstan is developing a platform to allow for off-the-shelf, targeted delivery of RNA to the desired cells or organs. It’s a broad enough platform to be applicable in cancer, genetic diseases, fibrosis and autoimmune diseases, like lupus.)
“I personally can’t even think of a therapeutic application of mRNA if their discovery hadn’t happened,” said Priya Karmali, Capstan’s chief technology officer. “Drew is a scientist to the core. What he really, really cares about is how one can translate the discoveries being done in his lab and others in the field into the future of human health.”
One day, for example, Weissman imagines a child receiving a single shot containing mRNA vaccines that protect against multiple diseases, all delivered with one lipid nanoparticle.
Karmali concludes: “He’s a visionary for thinking of the applications of this field beyond where we are today.”
Thank you to Kira Peikoff for additional research and reporting on this article.
Read the full article here