Only 15% of patients prescribed GLP-1s for weight loss were still taking the medications two years later, according to an analysis of pharmacy claims posted on July 10th by the pharmacy benefit manager, Prime Therapeutics. A flurry of other studies published recently show relatively high percentages of patients dropping out as early as four weeks into treatment and that discontinuation increases over time. Evidence that many people may stop their use of obesity drugs not long after starting therapy casts doubt about the sustainability of weight loss to achieve long-term positive health outcomes.
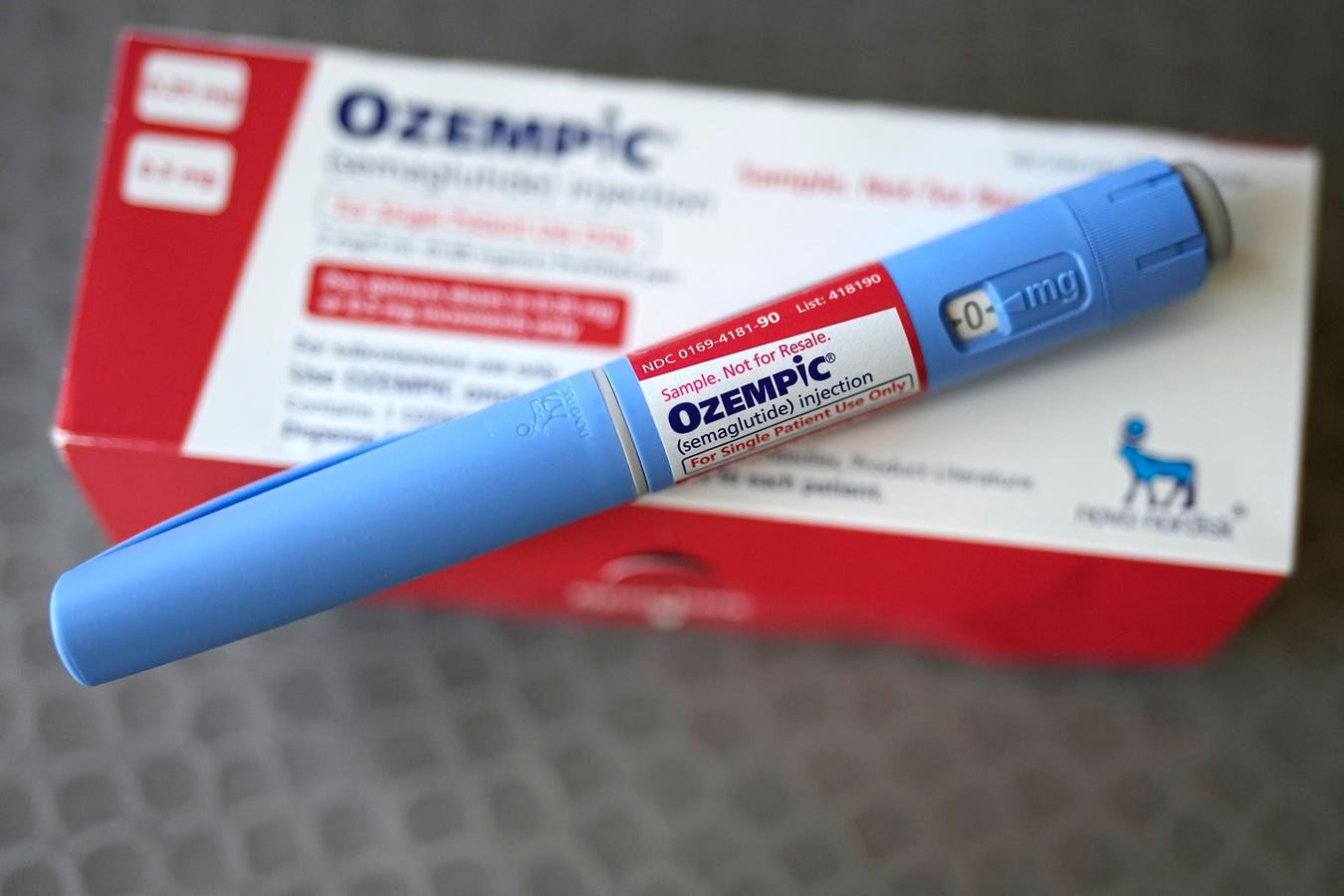
There is high demand for obesity medications known as glucagon-like peptide-1 agonists, or GLP-1s. In conjunction with an appropriate diet and exercise regimen, GLP-1s can provide substantial health benefits to patients. These aren’t confined to weight loss. GLP-1s have been used for almost two decades in the treatment of Type 2 diabetes. And a GLP-1 named Wegovy secured a supplemental cardiovascular indication from the Food and Drug Administration this spring.
The medications are also being studied in late stages of clinical development for chronic kidney disease and non-alcoholic fatty liver disease, where they’ve shown promise.
To attain these health benefits, however, it is critical that people prescribed GLP-1s continue to take them at least long enough to realize clinical success, and preferably longer to avoid possible weight rebound once they come off the medications.
The PBM Prime Therapeutics posted a new analysis on July 10th which shows that only about 15% of individuals who began taking GLP-1 drugs for weight loss persisted after two years.
Endpoints News reports that the PBM conducted an insurance claims analysis of 3,364 obese patients (body mass index greater than 30) who had started taking a GLP-1 during 2021 and were continuously enrolled with a commercial insurer. Patients with diabetes were excluded from the study.
Only 47% of patients were still taking a GLP-1 at 180 days; 29% at one year; and 15% at two years.
The drugs included in the study were Victoza (liraglutide), Saxenda (liraglutide), Ozempic (semaglutide) and Wegovy (semaglutide). Saxenda and Wegovy have weight loss indications approved by the Food and Drug Administration. Victoza and Ozempic are FDA-approved for diabetes and can be prescribed off-label for obesity.
Patients taking Ozempic and Wegovy—injected once-weekly—were more persistent than those on Victoza and Saxenda. About 24% using Wegovy were still on the drug at the two-year mark and 22% were continuing to take Ozempic.
Merely 7% of patients prescribed Victoza and Saxenda—injected once-daily—were taking them after two years.
The Prime Therapeutics study did not delve into reasons why patients quit the drugs. These can range from side effects to supply shortages. It could also be that patients had met their weight goal.
However, in a separate study posted by The Blue Cross Blue Shield Association last month, 58% of patients discontinue use before reaching a clinically meaningful level of weight loss. Notably, more than 30% of patients dropped out of treatment after the first month.
Also, a peer-reviewed study published by earlier this year by the research journal Obesity indicates that only 40% of obese patients taking semaglutide-based GLP-1 products were persistent at one year. And another refereed study released earlier this year by the Journal of Managed Care & Specialty Pharmacy revealed that 72% of individuals who started on GLP-1s for obesity were no longer taking them after one year.
These findings pose challenges for insurers and employers who make decisions whether to cover the drugs. If patients discontinue therapy, that can lead to weight rebound and ultimately a waste of resources, not only for the patient but also the payer. Wegovy and similar medicines are listed at more than $1,000 per month, NBC News notes, and may require extended use to produce meaningful benefits.
A recent survey conducted in late May of this year shows that just 34% of United States employer health plans offer coverage of GLP-1 drugs for both diabetes management and weight loss.
The lead author of the latest study—Patrick Gleason, Assistant Vice President, Health Outcomes at Prime Therapeutics—said in an interview with Endpoint News that the real-world data underscore the need for health plans to ensure patients receive comprehensive care, such as case and disease management programs aimed at behavior modification.
Citing limitations in the study, Novo Nordisk, which makes the drugs included in the claims analysis, said in a statement reported by Reuters that it “does not believe these data are sufficient to draw conclusions about overall patient adherence and persistence to various GLP-1 medicines, including our treatments.”
Nonetheless, the problem of lack of patient persistence on GLP-1s under real-world conditions, examined and published by a growing number of sources, isn’t going away. It will have to be addressed comprehensively by multiple stakeholders in order to improve the chances of achieving sustainable positive health outcomes for people trying to lose weight.
Read the full article here